Lisette Jacobson, Ph.D., MPA, M.A., using past Lauren S. Aaronson Pilot Award to Further Research Career in Helping to Improve Health in Rural and Urban Areas
By Kelly Hale , Marketing & Communications Specialist
Dec 05, 2024
When Lisette Jacobson, Ph.D., MPA, M.A., applied for Frontiers Lauren S. Aaronson Pilot Award in 2014, she had no idea how it would impact her research career.
“The pilot award really kicked off my research career and helped me develop my research agenda,” she said. “It led to a five-year K01 award from NIDDK. Applying for the pilot award helped show me what I needed for the K01. I also have a grant from the Kansas Center for Metabolism and Obesity Research (KC-MORE) to help gather additional data for the pilot intervention started under my K01.”
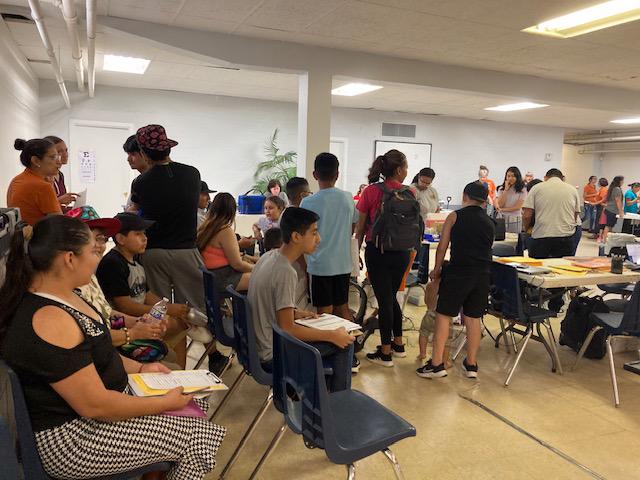
She was a key part of developing Pioneer Baby, which was a collaboration between the University of Kansas School of Medicine-Wichita, Ascension Health, and Kearny County Hospital (located about 25 miles west of Garden City, Kan.), a program to help improve pregnancy and birth outcomes. Doctors at the hospital were delivering babies from 12 counties at the time and the critical access facility was steadily bolstering its obstetrics capabilities. Jacobson collaborated with other doctors to help implement a program that helped pregnant women in rural areas who were at a higher risk for gestational diabetes during their pregnancy.
“When the program first started, they were seeing maybe 200 births a year, but that has grown to over 350 births a year from about 15 counties,” she said. “When we established Pioneer Baby, the gestational diabetes rate for this area was around 14% and the national average was around six or seven percent.”
(For more information on Pioneer Baby, click here.)
And as she continued to work in the areas of maternal and rural health, her Frontiers’ pilot award resulted in the publication of a peer-reviewed paper on stroke and breastfeeding in the Journal of the American Heart Association. The Journal, which is worldwide, led to Jacobson being interviewed nine times by national media. And the news release on the research led to 216 stories and more that 545 million media impressions according to the American Heart Association’s media relations team.
The article highlighted the impact of breastfeeding on maternal health outcomes, including potentially lowering the chance of stroke depending on other risk factors. The research in the article was critical to the areas of breastfeeding, lactation, and long-term cardiovascular health.
“Working on this paper really helped me establish connections across the US for possible collaborations,” she said. “I worked with a biostatistician from Ohio State through the Women’s Health Initiative as I worked on studying stroke among postmenopausal women and breastfeeding.”
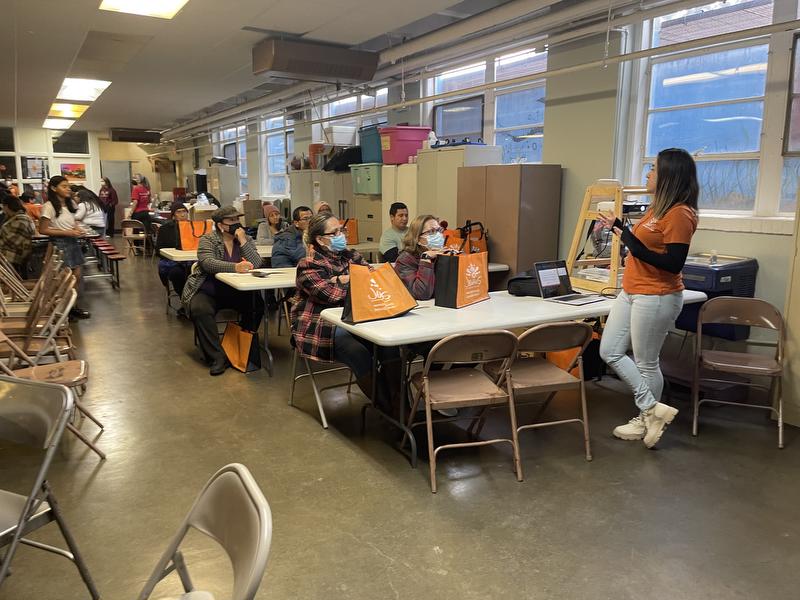
While working on her K01 award, Jacobson also developed eMOMSTM (electronic Monitoring of Mom’s Schedule), which was designed to improve postpartum weight, blood sugars and breastfeeding among women with high pre-pregnancy body mass index (BMI). Research had shown that longer durations of breastfeeding among women with gestational diabetes is associated with a lower risk to develop type 2 diabetes after pregnancy. The eMOMSTM program was modelled after the evidence-based national Diabetes Prevention Program (DPP) and coupled with breastfeeding education and support delivered via Facebook by a certified health coach.
Jacobson’s work under her K01 led to her current project working on a digital, mobile health (mHealth) application (app) of the eMOMSTM intervention. She continues to gather additional data to further the six-month intervention program, which currently includes not only participants in Kansas, but Florida, Texas, and Arkansas (the project is funded through a Women’s Health supplement from KC-MORE). The entirely digital program allows not only participants from other areas to join (if they meet the criteria), but also allows busy moms to work through the program at times that work for them.
“It’s really important to support moms after pregnancy too, but so many programs end at the end of pregnancy,” Jacobson, who has also served on the Kansas Rural Health Council for a few years, said. “After delivery and during the postpartum period, you can see morbidity and mortality rates rise without the support.”
She is also making the breastfeeding component of the eMOMSTM intervention a standalone project as she works with ECHO ISPCTN (Environmental Influences on Child Health Outcomes IDeA States Pediatric Clinical Trials Network), which brings innovative trials to medically under-served families, largely in rural areas but also in urban areas.
In addition, she is working on two policy statements around rural health across the US, specifically access to obstetrical and gynecological care for women in rural areas, and workforce issues in rural health. And, she will speak at the University of Arkansas Medical School Translational Research Institute next June.
“We’re in one of the most technologically advanced countries in the world and we have a high infant mortality rate and a high maternal morbidity and mortality rate,” she said. “Women in rural areas are continuing to have high risk pregnancies and some can’t get to the hospital in time to give birth. We must continue to work on this issue.”
And Jacobson credits her mentors for helping her throughout her career, while she has begun mentoring graduate students and medical school students both on the KU Medical School Wichita and Kansas City campuses. Her work, which started with a Frontiers Lauren S. Aaronson Pilot Award, is making an impact on maternal and rural health.
Latest Articles
View All Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Events
Events
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News

 TL1 Trainee · News
TL1 Trainee · News
 Services · News
Services · News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 KL2 Scholar
KL2 Scholar
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 News · In the Community · Funded Projects
News · In the Community · Funded Projects
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 Events · News
Events · News
 Funded Projects · News
Funded Projects · News

 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 News · In the Community · Funded Projects
News · In the Community · Funded Projects
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · News
KL2 Scholar · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 Events · News
Events · News

 KL2 Scholar · News
KL2 Scholar · News
 News
News
 Funded Projects · News
Funded Projects · News
 News
News
 Partner News · News
Partner News · News
 News · In the Community
News · In the Community

 0
0

 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Events · News
Events · News
 TL1 Trainee · News
TL1 Trainee · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 Funded Projects · News
Funded Projects · News
 News
News
 Partner News · News
Partner News · News
 TL1 Trainee · News
TL1 Trainee · News
 Events · News
Events · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News · KL2 Scholar
News · KL2 Scholar

 TL1 Trainee · News
TL1 Trainee · News
 Events · News
Events · News
 News
News
 News
News

 News
News

 40
40

 News
News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 Funded Projects · News
Funded Projects · News
 News · In the Community
News · In the Community
 Funded Projects · News
Funded Projects · News
 In the Community
In the Community
 News · In the Community · Partner News
News · In the Community · Partner News
 KL2 Scholar · News
KL2 Scholar · News
 News · In the Community
News · In the Community
 Events · News · Services
Events · News · Services
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · Funded Projects · News
KL2 Scholar · Funded Projects · News
 TL1 Trainee · Funded Projects · News
TL1 Trainee · Funded Projects · News
 News
News
 News
News
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 Events · News
Events · News
 News
News
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 News
News
 Funded Projects
Funded Projects

 TL1 Trainee
TL1 Trainee
 News
News
 Funded Projects
Funded Projects