Ana S.A. Cohen, Ph.D., FACMG - Investigating How to Expand Genetic Testing for Rare Diseases in Rural Areas
By Kelly Hale , Marketing & Communications Specialist
Apr 25, 2024
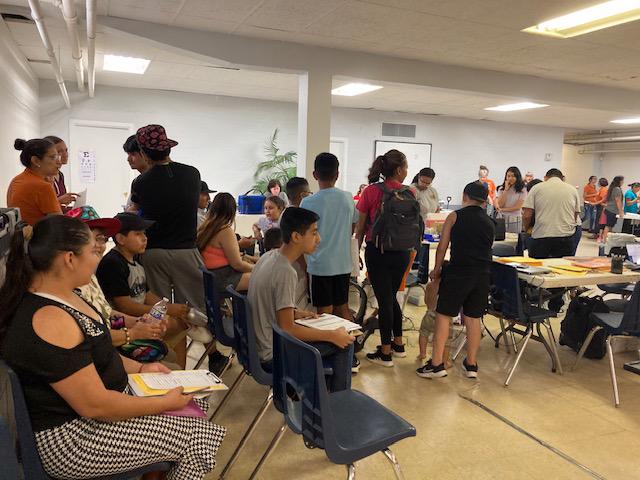
Individuals with undiagnosed rare genetic disorders face a long, challenging road to obtain a molecular diagnosis. Waitlists to see a specialist to initiate testing are at a minimum of six months due to a shortage of genetics specialists across the country. Further delays may occur post-consult due to insurance denials and/or restrictive testing. Families living in rural areas face even more challenges as the few specialists that are available tend to concentrate in large urban academic centers, meaning they must also overcome geographical isolation and reduced resources.
Investigator Ana Cohen, Ph.D., FACMG, an Assistant Director of Molecular Genetics at Children’s Mercy Kansas City, wanted to find ways to help families potentially get answers faster, while also trying to alleviate the burden of long travel time for those living in rural areas. She was able to explore this research with a Lauren S. Aaronson Pilot Award from Frontiers in 2022, working with a primary care clinic in Salina, Kansas (approx. 172 miles from Children’s Mercy). In the pilot project framework, the primary care providers were able to: initiate the genetic testing process, send patients’ samples to Dr. Cohen’s team at the Children’s Mercy Research Institute (within the Genomic Answers for Kids program) to process the test, and then receive the results back without the patients and families having to travel the distance to see a specialist in person pre-test.
“One of the primary care providers we worked with in Salina had trained at Children’s Mercy and was familiar with the process, which helped us establish this collaboration,” Cohen said. “For the families in Salina, this kept them from spending six to nine months on the waitlist then driving at least four hours just to initiate testing, and for a subset of them we reached a diagnosis in under four months!”
The initial results from the pilot study were positive, showing that participants had the same diagnostic rate as patients that would have gone through the traditional referral process and seen a specialist in-person, except that they received the results much faster given that they virtually skipped the waitlist. Importantly, this could not have happened without the structural support of the Genomic Answers for Kids program for test logistic processes and counselling pre- and post-test, as well as that of the Clinical Genetics staff at Children’s Mercy.
“Our clinical specialists have been really helpful through this process by helping support the primary care providers in recognizing which patients actually would benefit the most from genomic testing,” she said.
One important lesson learned was that these families also face more barriers in access to care post-test, often due to lack of appropriate resources for follow-up care in rural areas.
“Unfortunately, getting a molecular diagnosis is just one step in their long road. Though important, it does not solve most challenges that these families face,” Cohen said. “A lot of work and new partnerships will be needed to begin addressing this.”
Next steps for Cohen and her team include developing strategies to address post result support for the families and seeking funding to expand the program to more rural clinics.
Latest Articles
View All Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Events
Events
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News

 TL1 Trainee · News
TL1 Trainee · News
 Services · News
Services · News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 KL2 Scholar · News
KL2 Scholar · News
 Funded Projects · News
Funded Projects · News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 KL2 Scholar
KL2 Scholar
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 News · In the Community · Funded Projects
News · In the Community · Funded Projects
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 Funded Projects · News
Funded Projects · News
 Events · News
Events · News
 Funded Projects · News
Funded Projects · News

 Funded Projects · News
Funded Projects · News
 TL1 Trainee · News
TL1 Trainee · News
 News · In the Community · Funded Projects
News · In the Community · Funded Projects
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · News
KL2 Scholar · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 KL2 Scholar · News
KL2 Scholar · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 News
News
 Funded Projects · News
Funded Projects · News
 Events · News
Events · News

 KL2 Scholar · News
KL2 Scholar · News
 News
News
 Funded Projects · News
Funded Projects · News
 News
News
 Partner News · News
Partner News · News
 News · In the Community
News · In the Community

 0
0

 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Funded Projects · News
Funded Projects · News
 Funded Projects · News
Funded Projects · News
 News
News
 Events · News
Events · News
 TL1 Trainee · News
TL1 Trainee · News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 Funded Projects · News
Funded Projects · News
 News
News
 Partner News · News
Partner News · News
 TL1 Trainee · News
TL1 Trainee · News
 Events · News
Events · News
 KL2 Scholar · News
KL2 Scholar · News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News · KL2 Scholar
News · KL2 Scholar

 TL1 Trainee · News
TL1 Trainee · News
 Events · News
Events · News
 News
News
 News
News

 News
News

 40
40

 News
News
 News
News
 TL1 Trainee · News
TL1 Trainee · News
 News
News
 Funded Projects · News
Funded Projects · News
 News · In the Community
News · In the Community
 Funded Projects · News
Funded Projects · News
 In the Community
In the Community
 News · In the Community · Partner News
News · In the Community · Partner News
 KL2 Scholar · News
KL2 Scholar · News
 News · In the Community
News · In the Community
 Events · News · Services
Events · News · Services
 Funded Projects · News
Funded Projects · News
 KL2 Scholar · Funded Projects · News
KL2 Scholar · Funded Projects · News
 TL1 Trainee · Funded Projects · News
TL1 Trainee · Funded Projects · News
 News
News
 News
News
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 Events · News
Events · News
 News
News
 KL2 Scholar · Funded Projects
KL2 Scholar · Funded Projects
 News
News
 Funded Projects
Funded Projects

 TL1 Trainee
TL1 Trainee
 News
News
 Funded Projects
Funded Projects